CBDV, or cannabidivarin, is a shortened CBD molecule with a similar set of potentially additive benefits: anti-convulsive, antianxiety, anti-inflammatory, antiemetic, anti-itching, neuroprotective, and pain-relieving.
Like CBD, CBDV can also increase our endocannabinoids by slowing down certain enzymes and restoring endocannabinoid tone to alleviate symptoms of Rett syndrome, autism, and more. In fact, CBDV is orphan-designated by the European Medicine Agency (EMA) for Rett and Fragile X syndromes to address brain inflammation and seizures.
CBDV hits many other non-ECS targets, including dopamine actions that could lend well for various neurodegenerative and psychiatric disorders. Common side effects include diarrhea, nausea, and drowsiness.
What Is CBDV?
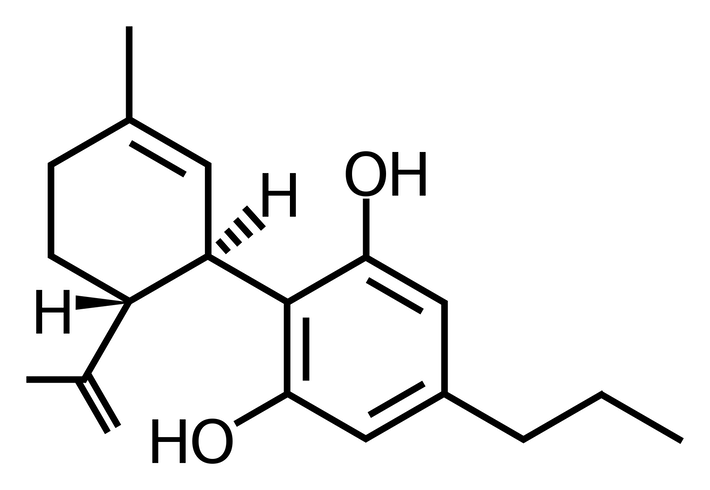
Before CBDV was found in 1969, scientists thought that all natural cannabinoids must have a 5-carbon tail. Then, CBDV appeared with only 3 carbons and changed that notion.
Ever since, CBDV has been on the rise as a minor cannabinoid mimicking CBD. A “minor” cannabinoid is one that is naturally found in relatively small amounts and so must be extracted into oils, edibles, vapes, and more. Limited data suggest CBDV may have a surprisingly further clinical reach.
Specifically, there is increasing interest in CBDV to treat neuropsychiatric or pain conditions that are not adequately treated by Western medicine or other cannabinoids. The scope of this research is broad and ongoing.
Currently, it includes seizures (adult and pediatric), autism spectrum disorder, Rett syndrome, Fragile X syndrome, Duchenne muscular dystrophy, and chronic pain.
CBDV vs. THC: Key Differences
- Separate molecules with distinct structures
- Unlike THC, CBDV is non-intoxicating and non-hallucinogenic
- Both may be used for nausea, but CBDV comes without psychoactivity
- THC increases appetite, while CBDV may reduce it
CBDV vs. CBD: Key Differences
- CBDV is 2 carbons shorter than CBD, allowing unique receptor interactions
- CBDV and CBD share many properties, best known for its anti-epileptic, neuroprotective, non-intoxicating, well-tolerated, and anti-inflammatory features
- Both may increase endocannabinoid tone and cause similar medication interactions
- CBD and CBDV may be additive in epilepsy, but only CBD is FDA-approved in the US while CBDV is an orphan drug approved by the EMA
What Are the Benefits and Effects of CBDV?
We are only beginning to understand the possible benefits and effects of CBDV through limited clinical and animal trials. However, the data are promising enough to warrant further rigorous clinical research in:
- Seizures in adult epilepsy, and childhood Fragile X and Rett syndromes
- Autism symptoms, with mice having improvements in ECS signaling, memory deficits, cognitive deficits, social impairments, motor coordination, movement, and brain weight
- Nausea, alleviated in mice
- Duchenne muscular dystrophy, where CBDV improved mice muscle quality and movement while slowing degeneration and inflammation
- Ulcerative colitis and associated intestinal inflammation may be mitigated, along with better-regulated gut microbiota
- Chronic pain through many non-ECS pathways, and may reduce opioid dosing
What Are the Side Effects of CBDV?

CBDV is considered generally well-tolerated. In a phase II clinical study of epileptic adults, CBDV had mostly mild-to-moderate side effects that were more frequent than placebo. From most to least commonly reported, these include:
- Diarrhea
- Drowsiness
- Nausea
- Headache
- Dizziness
- Upper abdominal pain
- Rash
- Decreased appetite
Unexpectedly, there are reports of serious adverse effects including intoxication, altered mental status, and lab abnormalities (e.g., transaminitis, azotemia). It is unclear whether CBDV alone, medication interactions, or something else played a role in these cases. In a pediatric study, experts found that serious events were related to the underlying disease (RTT).
CBDV inhibits many enzyme families and may raise levels of medications like warfarin, antidepressants, statins, antiepileptics, and more. The clinical significance of this is yet unclear, but talking to your doctor is important before starting CBDV.
Overall lack of effects on vital signs (e.g., heart rate, etc.), physical exam, ECGs, and no production of withdrawal or suicidal thoughts are also critical to note for assessing general safety and tolerability.
How Much CBDV Should You Take?

If you’re interested in starting CBDV, you or a loved one probably have a chronic or serious neuropsychiatric illness that already requires ongoing healthcare provider consultation. The dosage you should start with CBDV depends on your age, condition, and access.
Currently, the EMA has not issued guidelines for CBDV dosing as an orphan drug.
Note that in a recent clinical trial, the average daily dose was 1480 mg of purified CBDV for epileptic adults. However, such extremely high doses are done with exploratory intentions and are probably not necessary for everyday wellness or for managing the symptoms of your condition.
A small 2022 study started titrating CBDV at 2.5 mg/kg/day and found a dose of 10 mg/kg/day was safe and effective for seizure control in pediatric Rett syndrome patients. This is similar dosing to Epidiolex® (pharmaceutical CBD).
Still, generalizable and further specific data just isn’t there yet. Working closely with your specialists and a cannabis coach may be helpful in determining what is most suitable.
Will CBDV Get You High?
No, CBDV should not get you high. It is theorized that enough CBDV could stimulate CB1 – but this is not shown to cause a high in animals or humans. The absence of withdrawal symptoms in clinical studies supports this.
You can watch Dr. Benavides and his team at GW CIM discussing the clinical uses of CBDV in the video below.
Will CBDV Show Up on a Drug Test?
Possibly, yes. If your CBDV is in a typical full-spectrum formulation, then over time the small amount of legal THC in hemp can accumulate and compromise drug testing results.
RELATED: CBD and Drug Tests: Everything You Need to Know
Taking broad-spectrum (“THC-free”), or purified or isolated CBDV may prevent this, but may also be less effective this way.
Conclusion
CBDV presents itself as a wonderful compliment to the well-known CBD, both on its own and in synergy. CBDV could be a missing, key component to treating many complex neuropsychiatric and pain conditions.
This limited research opens our eyes to new possibilities for helping people’s suffering insufficiently addressed by modern medicine or even CBD alone.
References (22)
- Babayeva, M., Assefa, H., Basu, P., & Loewy, Z. (2022). Autism and associated disorders: Cannabis as a potential therapy. Frontiers in Bioscience-Elite, 14(1), Article 1. https://doi.org/10.31083/j.fbe1401001
- Brodie, M. J., Czapinski, P., Pazdera, L., Sander, J. W., Toledo, M., Napoles, M., Sahebkar, F., & Schreiber, A. (2021). A Phase 2 Randomized Controlled Trial of the Efficacy and Safety of Cannabidivarin as Add-on Therapy in Participants with Inadequately Controlled Focal Seizures. Cannabis and Cannabinoid Research, 6(6), 528–536. https://doi.org/10.1089/can.2020.0075
- Hurley, E. N., Ellaway, C. J., Johnson, A. M., Truong, L., Gordon, R., Galettis, P., Martin, J. H., & Lawson, J. A. (2022). Efficacy and safety of cannabidivarin treatment of epilepsy in girls with Rett syndrome: A phase 1 clinical trial. Epilepsia, 63(7), 1736–1747. https://doi.org/10.1111/epi.17247
- Wang, X., Lin, C., Wu, S., Zhang, T., Wang, Y., Jiang, Y., & Wang, X. (2022). Cannabidivarin alleviates neuroinflammation by targeting TLR4 co-receptor MD2 and improves morphine-mediated analgesia. Frontiers in Immunology, 13. https://www.frontiersin.org/articles/10.3389/fimmu.2022.929222
- Walsh, K. B., McKinney, A. E., & Holmes, A. E. (2021). Minor Cannabinoids: Biosynthesis, Molecular Pharmacology and Potential Therapeutic Uses. Frontiers in Pharmacology, 12, 777804. https://doi.org/10.3389/fphar.2021.777804
- Farrelly, A. M., Vlachou, S., & Grintzalis, K. (2021). Efficacy of Phytocannabinoids in Epilepsy Treatment: Novel Approaches and Recent Advances. International Journal of Environmental Research and Public Health, 18(8), 3993. https://doi.org/10.3390/ijerph18083993
- Benavides, A. (2022, January 24). Cannabinoids and the Endocannabinoid System: A Match Made in Heaven. Doctor’s Corner. https://www.veriheal.com/blog/cannabinoids-and-the-endocannabinoid-system-a-match-made-in-heaven/
- Dr. Misha Kogan (Director). (2023, March 24). CBDV – Cannabidivarin, Acute on Chronic and GWCIM Virtual Open House. https://www.youtube.com/watch?v=7_vR1vU8n4I
- Eibach, L., Scheffel, S., Cardebring, M., Lettau, M., Özgür Celik, M., Morguet, A., Roehle, R., & Stein, C. (2021). Cannabidivarin for HIV-Associated Neuropathic Pain: A Randomized, Blinded, Controlled Clinical Trial. Clinical Pharmacology & Therapeutics, 109(4), 1055–1062. https://doi.org/10.1002/cpt.2016
- Shrader, S. H., Tong, Y.-G., Duff, M. H., Freedman, J. H., & Song, Z.-H. (2020). Involvement of Dopamine Receptor in the Actions of Non-Psychoactive Phytocannabinoids. Biochemical and Biophysical Research Communications, 533(4), 1366–1370. https://doi.org/10.1016/j.bbrc.2020.10.021
- Di Marzo, V. (2020). The endocannabinoidome as a substrate for noneuphoric phytocannabinoid action and gut microbiome dysfunction in neuropsychiatric disorders. Dialogues in Clinical Neuroscience, 22(3), 259–269. https://doi.org/10.31887/DCNS.2020.22.3/vdimarzo
- Alves, P., Amaral, C., Teixeira, N., & Correia-da-Silva, G. (2020). Cannabis sativa: Much more beyond Δ9-tetrahydrocannabinol. Pharmacological Research, 157, 104822. https://doi.org/10.1016/j.phrs.2020.104822
- DrugBank Online. (2020, June 8). Cannabidivarin. https://go.drugbank.com/drugs/DB14050
- Morano, A., Fanella, M., Albini, M., Cifelli, P., Palma, E., Giallonardo, A. T., & Di Bonaventura, C. (2020). Cannabinoids in the Treatment of Epilepsy: Current Status and Future Prospects. Neuropsychiatric Disease and Treatment, 16, 381–396. https://doi.org/10.2147/NDT.S203782
- Pagano, E., Romano, B., Iannotti, F. A., Parisi, O. A., D’Armiento, M., Pignatiello, S., Coretti, L., Lucafò, M., Venneri, T., Stocco, G., Lembo, F., Orlando, P., Capasso, R., Di Marzo, V., Izzo, A. A., & Borrelli, F. (2019). The non-euphoric phytocannabinoid cannabidivarin counteracts intestinal inflammation in mice and cytokine expression in biopsies from UC pediatric patients. Pharmacological Research, 149, 104464. https://doi.org/10.1016/j.phrs.2019.104464
- Pretzsch, C. M., Voinescu, B., Lythgoe, D., Horder, J., Mendez, M. A., Wichers, R., Ajram, L., Ivin, G., Heasman, M., Edden, R. A. E., Williams, S., Murphy, D. G. M., Daly, E., & McAlonan, G. M. (2019). Effects of cannabidivarin (CBDV) on brain excitation and inhibition systems in adults with and without Autism Spectrum Disorder (ASD): A single dose trial during magnetic resonance spectroscopy. Translational Psychiatry, 9(1), Article 1. https://doi.org/10.1038/s41398-019-0654-8
- Zamberletti, E., Gabaglio, M., Woolley-Roberts, M., Bingham, S., Rubino, T., & Parolaro, D. (2019). Cannabidivarin Treatment Ameliorates Autism-Like Behaviors and Restores Hippocampal Endocannabinoid System and Glia Alterations Induced by Prenatal Valproic Acid Exposure in Rats. Frontiers in Cellular Neuroscience, 13, 367. https://doi.org/10.3389/fncel.2019.00367
- Iannotti, F. A., Pagano, E., Moriello, A. S., Alvino, F. G., Sorrentino, N. C., D’Orsi, L., Gazzerro, E., Capasso, R., De Leonibus, E., De Petrocellis, L., & Di Marzo, V. (2019). Effects of non‐euphoric plant cannabinoids on muscle quality and performance of dystrophic mdx mice. British Journal of Pharmacology, 176(10), 1568–1584. https://doi.org/10.1111/bph.14460
- Muller, C., Morales, P., & Reggio, P. H. (2019). Cannabinoid Ligands Targeting TRP Channels. Frontiers in Molecular Neuroscience, 11, 487. https://doi.org/10.3389/fnmol.2018.00487
- Stahl, S. M. (2017). Drugs for psychosis and mood: Unique actions at D3, D2, and D1 dopamine receptor subtypes. CNS Spectrums, 22(5), 375–384. https://doi.org/10.1017/S1092852917000608
- Iannotti, F. A., Hill, C. L., Leo, A., Alhusaini, A., Soubrane, C., Mazzarella, E., Russo, E., Whalley, B. J., Di Marzo, V., & Stephens, G. J. (2014). Nonpsychotropic Plant Cannabinoids, Cannabidivarin (CBDV) and Cannabidiol (CBD), Activate and Desensitize Transient Receptor Potential Vanilloid 1 (TRPV1) Channels in Vitro: Potential for the Treatment of Neuronal Hyperexcitability. ACS Chemical Neuroscience, 5(11), 1131–1141. https://doi.org/10.1021/cn5000524
- Rock, E. M., Sticht, M. A., Duncan, M., Stott, C., & Parker, L. A. (2013). Evaluation of the potential of the phytocannabinoids, cannabidivarin (CBDV) and Δ9-tetrahydrocannabivarin (THCV), to produce CB1 receptor inverse agonism symptoms of nausea in rats. British Journal of Pharmacology, 170(3), 671–678. https://doi.org/10.1111/bph.12322

